At this time, there is no way to prevent or cure either the dry (atrophic) or wet (neovascular) form of macular degeneration. However, significant progress has been made in treating the condition, and a great deal of research is currently under way. The most significant advance has been the development of a new class of drugs now being used to treat wet macular degeneration. The drugs are based on the discovery that a group of proteins in the body, called vascular endothelial growth factor (VEGF), play a significant role in the formation of the abnormal blood vessels that damage the retina in wet macular degeneration. These abnormal blood vessels are called choroidal neovascularization (CNV).
The anti-VEGF drugs are injected directly into the jelly-like substance that fills the back of the eye, which is called the vitreous. Before the injection, drops are used to numb the eye and a speculum may be put in place to hold the eyelids out of the way. While it may seem scary to receive an injection into the eye, most patients find that they experience minimal discomfort. Once inside the eye, the medication diffuses throughout the retina and choroid. It binds strongly to the abnormal VEGF proteins, preventing the proteins from stimulating further unwanted blood vessel growth and leakage.
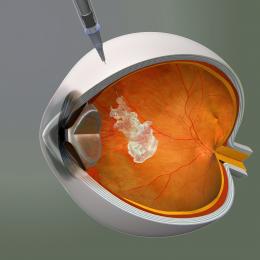

Before injection of an anti-vascular endothelial growth factor (VEGF) drug, the eye is numbed and a speculum may be put in place to keep the eyelids out of the way.
Two anti-VEGF drugs have been approved by the U.S. Food and Drug Administration (FDA) for the treatment of wet macular degeneration. The one most widely used is Lucentis (ranibizumab). In the studies that evaluated Lucentis, the results were more favorable than for any other previously FDA approved treatment. Instead of only slowing the rate of vision loss, the drug appeared to stop disease progression in most people for as long as two years. Also, many patients in the study gained a small amount of vision, and some experienced significant improvement.
It is important to note that the patients in the study had fairly recently diagnosed macular degeneration that had not yet progressed to scarring. Each person responds differently to treatment, depending on his or her individual situation. In the studies of Lucentis, patients were given injections every month for up to two years. More recent evidence suggests that it may be possible to obtain similar results by giving several injections at monthly intervals and then increasing the time between subsequent injections. Retinal specialists are still investigating the optimal timing of injections. Also, research is under way to develop other methods of delivering drugs to the eye to reduce the need for frequent injections.
The first anti-VEGF drug to be approved by the FDA for the treatment of wet macular degeneration was Macugen (pegaptanib sodium). It works in a similar manner to Lucentis, but is not as effective. This is most likely because it acts against only one form of the VEGF protein, called VEGF-165, whereas Lucentis targets all forms of VEGF.
In theory, if Lucentis from the eye were to travel to other parts of the body and interfere with VEGF, it could lead to problems, such as an increased risk of heart attack or stroke. However, the amount of drug injected is small, and no safety problems have emerged with the use of Lucentis.
Your ophthalmologist will explain the advantages and disadvantages of all available treatments for wet macular degeneration and choose your treatment based on your individual case. The FDA-approved anti-VEGF drugs are costly, but the pharmaceutical companies that make them offer assistance programs for patients who qualify. Ask your ophthalmologist for information about these programs.